Biological Age Testing Explained: DNA Methylation Clocks, Telomeres, and What Organ Age Really Means

By Danielle Ruiz, MSN, APRN, AGNP-C
Aging is inevitable. But the speed at which we age biologically is far more variable—and far more modifiable—than the number printed on a driver’s license.
Chronological age simply counts the years since you were born. Biological age reflects how well your body is actually functioning—how resilient your cells are, how efficiently your organs repair damage, and how effectively your systems maintain balance over time.
Two people can both be 55 years old chronologically, yet one may have the cardiovascular flexibility, metabolic stability, and cellular repair capacity of someone in their 30s, while the other shows biological patterns more typical of someone approaching 70. The difference is not random. It is the cumulative result of genetics, lifestyle, environment, and increasingly, the interventions we choose to adopt.
What makes this moment in medicine so compelling is that biological aging is now measurable. Biological age tests allow physicians to estimate aging speed with increasing accuracy—and those measurements are proving to be stronger predictors of health outcomes than chronological age alone.
What Is Biological Age?
Biological age represents the functional condition of your cells, tissues, and organs. Unlike chronological age, it is dynamic and responsive to lifestyle, medical care, and metabolic health.
Research consistently shows that people whose biological age exceeds their chronological age face higher risks of:
- Cardiovascular disease
- Cancer and metabolic disorders
- Cognitive decline and frailty
- Earlier mortality
When biological age is lower than chronological age, the opposite tends to be true: stronger organ function, greater stress resilience, and longer healthspan.
In practical terms, biological age serves as an early warning system. A sudden increase may reflect inflammation, sleep deprivation, stress, or illness. A gradual decrease often mirrors successful lifestyle and medical intervention.
Rather than guessing how someone is aging, modern medicine can now measure it.
How Biological Age Is Measured
There is no single biological age test. Clinicians rely on several complementary approaches that examine aging from different biological perspectives.
DNA Methylation Clocks (Epigenetic Age Testing)
Epigenetic clocks analyze DNA methylation patterns—chemical markers on DNA that influence gene expression. These patterns change predictably with age and respond to environmental and lifestyle factors.
Blood or saliva samples are analyzed across hundreds to thousands of genomic sites and compared against population datasets to estimate epigenetic age.
Some clocks focus on chronological estimation, while newer second-generation clocks are better at predicting disease risk, frailty, and mortality. Importantly, epigenetic age responds to interventions such as improved nutrition, exercise, smoking cessation, stress reduction, and metabolic optimization.
Each standard deviation of epigenetic age acceleration is associated with approximately a 25 percent increase in mortality risk, making epigenetic clocks powerful clinical risk-assessment tools.
Metabolic Biological and Phenotypic Age
Phenotypic biological age is calculated from routine blood biomarkers reflecting inflammation, kidney function, glucose regulation, immune balance, and organ performance.
These tests often predict mortality and disability better than chronological age and are especially useful for tracking change over time. Hybrid clocks that combine epigenetic and metabolic markers data are emerging as some of the strongest predictors of long-term health outcomes.
Because these biomarkers change meaningfully with lifestyle and medical therapy, they are particularly useful for guiding and adjusting personalized interventions.
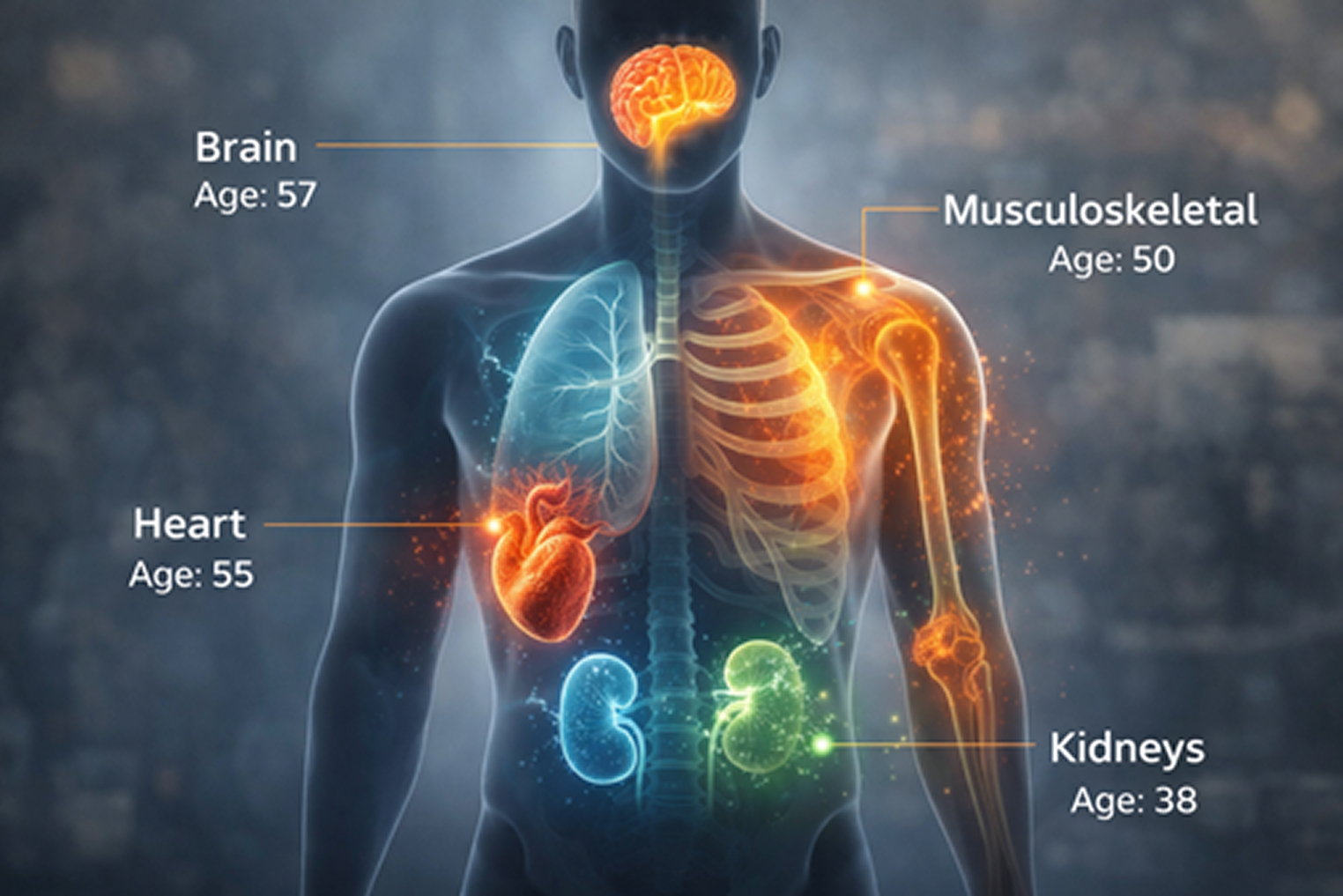
Organ-Specific Biological Age
Organs do not age uniformly.
A person may have an excellent overall biological age while showing accelerated aging in a single system such as the heart, kidneys, brain, or musculoskeletal system. That vulnerable organ often determines long-term health trajectory.
Organ-specific aging is assessed through imaging, laboratory trends, and functional testing. This transforms aging from an abstract concept into a personalized map of strengths and vulnerabilities.
Identifying which organs are aging fastest allows clinicians to target interventions precisely where they matter most.
Telomere Length Testing
Telomeres are protective caps at the ends of chromosomes that shorten with cell division. While shorter telomeres are associated with increased cardiovascular and mortality risk, telomere length alone correlates only modestly with functional aging.
Today, a telomere length test is best viewed as a marker of cumulative cellular stress rather than a primary driver of biological aging. It often disagrees with epigenetic and phenotypic clocks and provides less actionable clinical guidance for most patients.
How Often Should You Test Biological Age?
For individuals actively optimizing health, biological age testing every six to twelve months is generally sufficient. During major lifestyle or therapeutic changes, more frequent testing may be appropriate.
We typically recommend starting with a baseline and retesting every six months for most patients actively optimizing health. The most important factor is not the absolute number, but the trend over time and how those trends are interpreted in a clinical context.
Biological age testing becomes truly valuable when integrated with comprehensive laboratory analysis, functional and imaging assessments, personal medical history, and provider-guided interpretation.

Why Biological Age Testing Matters
Biological age testing represents one of the most important shifts in modern preventive and longevity medicine. It transforms aging from something we passively experience into something we can actively measure, monitor, and influence.
By combining epigenetic clocks, metabolic biomarkers, and organ-specific assessments, clinicians and patients can:
- Detect accelerated aging early
- Identify hidden health vulnerabilities
- Track real progress from changes
- Design truly personalized strategies
At Everest Health, biological age assessment is a foundational component of the Methuselah Protocol, integrating molecular, metabolic, and functional data into a comprehensive longevity strategy. The objective is not simply to extend lifespan, but to preserve vitality, independence, and performance across decades.
If you have ever searched for “biological age testing near me” or are simply curious about how quickly you are truly aging—and what can be done to influence it—biological age testing offers one of the clearest windows modern medicine has to offer. Click here to schedule a consultation and begin building a strategy for longer, healthier, and more resilient years ahead.
The future of longevity medicine is not about guessing. It is about measuring, understanding, and acting with precision.
This article reflects scientific understanding as of early 2026 and is intended for educational purposes only. Always consult a qualified healthcare professional before pursuing testing or intervention.
Related FAQs
What is biological age testing?
Biological age testing measures how well your body is functioning compared to your chronological age. It evaluates cellular health, metabolism, and organ function to estimate how quickly you’re aging biologically—not just how many birthdays you’ve had.
How is biological age measured?
Biological age is assessed using advanced tools such as DNA methylation (epigenetic) clocks, blood-based metabolic biomarkers, and organ-specific testing. These methods together provide a more accurate picture than any single test alone.
Can I lower my biological age?
Yes. Biological age is modifiable. Improvements in nutrition, exercise, sleep, stress management, and targeted medical interventions can slow—or even reverse—biological aging markers over time.
How often should biological age testing be done?
Most patients benefit from testing every 6–12 months. This allows enough time to see meaningful biological changes while tracking progress and adjusting interventions as needed.
Is telomere testing enough on its own?
No. While telomere length reflects cumulative cellular stress, it does not fully capture how your body is aging. Modern longevity assessments rely more heavily on epigenetic and metabolic markers for actionable insights.